Assisted Reproductive Technology
Summary of the female reproductive system
MESA (Microsurgical epididymal sperm aspiration)
Description
Sperm are retrieved directly from the epididymis (area in the testes where
sperm mature and are stored).
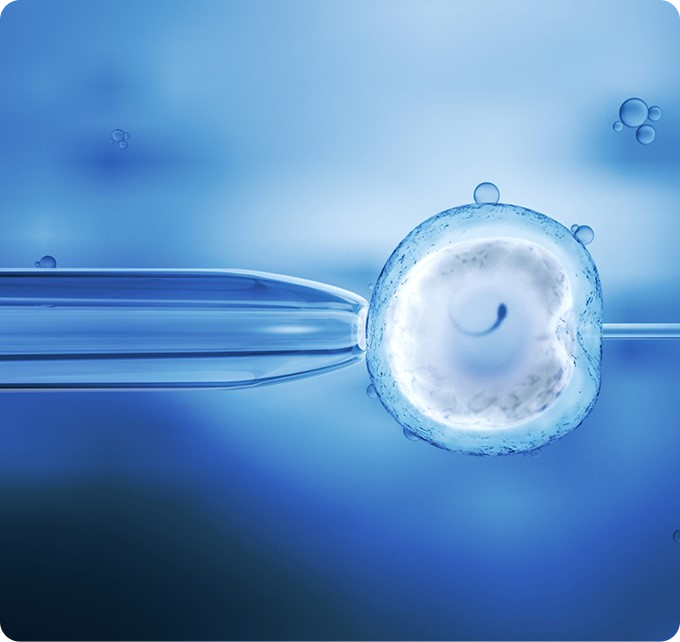
Fertilisation is then attempted with ICSI.
Function
Pear-shaped cavity containing endometrial tissue, and a lower port Severe male infertility. Absence of sperm in the ejaculate (azoospermia). Congenital abnormalities (e.g absence of vas deferens).ion called the cervix.
TESE (Testicular sperm extraction)
Description
Biopsy of the testes is performed in order to obtain sperm directly from testicular issue. Fertilisation is then attempted with ICS.
Function
Severe male infertility. Absence of sperm in epididymis. Absence of epididymis.
GIFT (Gamete intra-fallopian transfer)
Description
Follows same procedures as IVF except that fertilization occurs in the body (in vivo). Sperm and eggs are placed directly into the fallopian tubes where fertilization can occur.
Function
Infertility due to endometriosis and cervical mucus disorders. Religious reasons. Unexplained infertility. Some cases of male infertility.
Fallopian Tube
Description
Canal leading from outside of body to cervix.
Function
Serves as lower part of birth canal receives sperm from male.
ZIFT (Zygote intra-fallopian transfer)
Description
Same procedures as IVF except that fertilised eggs are placed in the fallopian tubes at a certain stage of embryo development (zygote).
Function
Same as for GIFT.
Investigations
Work Up Of Infertile Couples.
Couples come to FFC for their infertility treatments. The couple is evaluated by taking their detailed history, and examination is done by the team of experts to establish the cause of infertility. Further investigations and workup is planned according to the cause of infertility.
Semen Analysis
In most of the cases sperm count and motility are the main factors to be considered for fertilisation but this process also require normal sperms(morphologically) to form an embryo, though studies have also shown that an abnormally shaped sperm can also fertilise an egg but infertility is actually associated with higher amounts of abnormally shaped sperms. Sometimes this higher number of abnormally shaped sperms are also linked with other irregularities of semen such as low sperm count or motility.In short ,sperm morphology is also being used in some cases to decide whether a couple should attempt pregnancy or not.
A normal shaped sperm has following features
Have an oval head with a long tail.
Abnormal sperm have head or tail defects — such as a large head or a crooked or double tail.
These defects might affect the ability of the sperm to reach and penetrate an egg. … Total sperm number
Preliminary Testing – Semen Analysis (Cont)
The table below lists the World Health Organization (WHO) criteria for normal semen analysis. Which may be helpful when your doctor discusses your results.
Normal Semen Analysis WHO 2010.
Volume of semen
≥ 1.5 mL
Sperm concentration
≥ 15 x 106
Total motility (PR & NP)
≥ 40%
Morphological normal sperm
≥ 4%
Treating Options For Infertile Couples
A semen sample can reveal a real picture of sperms and certain hormone tests can also be done (in case ,they are required). By considering the test results, problems with male infertility are identified and treated according to the underlying cause.
On the other hand, a female history is also very helpful in order to know the following essential conditions which are required for pregnancy but may not be functioning correctly.
The right balance of hormones to allow egg and sperm development and support.
A mature female egg ( female oocyte or gamete) and whether ovulation regularly takes place.
The functioning reproductive tract ( uterus and Fallopian tubes) , which allows for the egg and sperm to meet and fertilise.
The ability of the female body to allow for implantation of an embryo and to maintain and nourish that embryo.
On the basis of the above finding female history, a specialist doctor may recommend certain Blood tests.
Hormonal Profile/ Ovulation Testing/ Hysterosalpinography
Following tests are performed to evaluate the levels of hormones that promote ovulation and implantation of the egg.
FSH- Responsible for stimulation of egg growth.
Luteinizing hormone (LH) – Responsible for egg release from the follicles.
Estradiol( E2) – Responsible for the stimulation of follicles.
Progesterone- Responsible for stabilisation of the uterine lining for egg implantation and pregnancy.
AMH (Anti Mullarian Hormone test)
The over production of certain hormones can adversely effect ovulation.
Androgen- In women excess production can hinder growth of follicles and ovulation.
Prolactin- Higher levels than normal causes certain disorders.
Thyroid- An under active thyroid can cause high levels of prolactin.
Hysterosalpingography
Hysterosalpingography is a radiologic procedure to help investigate the anatomical defects, of uterus , its cavity and patency of the fallopian tubes. A radio-opaque material is injected into the cervical canal to show the filling of the uterine cavity and the bilateral filling of the Fallopian tube. Afterwards series of x-rays are performed.
Transvaginal Ultrasound.
An ultrasound test which uses high-frequency sound waves to create images of internal organs. Imaging tests can identify abnormalities and help doctors diagnose conditions.
A transvaginal ultrasound also called an endovaginally ultrasound, is a type of pelvic ultrasound used by doctors to examine female reproductive organs. This includes the uterus, fallopian tubes, ovaries, cervix, and vagina.
HysterosalpingographyLaparoscopy
In the cases of infertility, once a detailed evaluation of the couple has been carried out, laparoscopy is a gold standard diagnostic investigation meant for.
Evaluating the female partner. With the help of diagnostic laparoscopy, a doctor is able to directly visualize the female pelvic organs.
It is helpful to see the whole genital tract. Vagina, cervix, uterus, Fallopian tubes, ovaries are directly visualized during the process.
Tubal patency is checked during laparoscopy.
Any ovarian pathology/ cyst is not directly visualized but can be treated with operative laparoscopy.
At the same time, Adhesiolysis can also be done during laparoscopy.
Clipping of the tubes is done with the help of a laparoscope in case of endometriosis prior to the IVF procedure.
How It Is Done?
It is a daycare procedure. It is performed under general anesthesia. The total duration for diagnostic laparoscopy is 13 minutes. And at least,
Six hours of NPO is required before performing the procedure.
After laparoscopy patient is kept under observation for 3-4 hours.
The patient usually requires 1-2 doses of post-operative analgesia.
The patient can be discharged on the same day.